Policy Update: The Ban on Corneal Transplant Donation for Men Who Have Sex with Men
Author: Whitney Stuard Sambhariya, MD, PhD
Referenced: Michael A. Puente, MD
Assistant Professor of Ophthalmology at the University of Colorado, Co-Founder of the American Academy of Ophthalmology (AAO) LGBTQ+ interest group, President of Colorado Society of Eye Physicians and Surgeons (CSEPS), and Chair of the American Association for Pediatric Ophthalmology & Strabismus (AAPOS) Legislative Committee
The Past
In 1994 the U.S. Public Health Service put into place a policy banning the use of tissues for transplantation from men who have had sex with men (MSM) within the past five years, a policy which has subsequently been adopted and enforced by the Food and Drug Administration (FDA).[1, 2]
This policy was implemented at a time when human immunodeficiency virus (HIV) was still a relatively new disease and there was concern about transmission through corneal transplantation.[3] Furthermore, there were no reliable ways to test donor tissues for the presence of the virus prior to transplantation.[4] Therefore, due to fear of spreading the disease via transplantation, and the lack of effective reliable testing for HIV, the policy was put in place.
In 2020, Puente et al. estimated that approximately 1,600 to 3,200 corneas are not deemed fit for transplant in the United States and Canada each year due to this policy and its Canadian equivalent.[5, 6] While this may not seem like an overwhelming number, there is only 1 cornea currently available for transplant for every 70 needed, leading to extensive waiting lists in many countries. Furthermore, there are over 12.7 million people worldwide who are impacted by this shortage.[7-9]
Since 1994, HIV detection methods have improved, with enzyme-linked immunosorbent assay (ELISA) and nucleic acid testing (NAT) becoming more prominent in the 2000s. Currently, every donor cornea intended for transplant undergoes three separate tests to detect HIV: ELISA HIV1, ELISA HIV2, and NAT HIV.[5] These tests have a 99% accuracy rate at identifying HIV within 4-8 days of exposure.[10, 11] Although there is a global scarcity of donor corneas, this policy results in the exclusion of corneas of MSM even if they test negative for HIV.
At present, this policy is now contrasting with evidence-based practice. MSM are still subjected to this policy, while heterosexual individuals with known HIV exposure are only subject to a one-year deferral period.[2] Interestingly, MSM are not banned from donating full organs, only tissue, which adds to the inconsistency in policy. Furthermore, there has never been a case of HIV transmitted through corneal transplantation even if the donor had HIV.[5, 12]
What is happening to help change this policy?
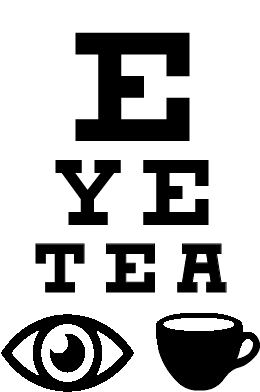
Ophthalmologist and policy advocate Dr. Michael Puente has emerged as a leader in the charge of “Legalize Gay Eyes” after encountering the story in 2019 of a gay teenager who committed suicide in 2013 due to homophobic bullying. The patient, an organ donor, was able to extend the lives of others as the policy above allowed for his organs to be transplanted, while his corneas, deemed a tissue, were not considered for transplantation because of his sexual orientation.[13] Dr. Puente worked to determine the impact of this policy by calling every eye bank in the United States and Canada to determine how many corneas were being discarded each year from otherwise eligible donors. The number, as stated above, is an impressive 1600-3200 corneas annually that could be used to cure blindness.[5]
The American Academy of Ophthalmology (AAO) took a stand against this policy in 2021 after a council advisory recommendation was submitted by Dr. Puente through the Colorado Society of Eye Physicians and Surgeons. Dr. Puente then submitted a similar resolution to the American Medical Association (AMA) through the Colorado Medical Association. After initially voting the policy down in 2021, AMA voted in 2022 to adopt Puente’s resolution, leading to AMA policy H-50.973, which states the AMA “opposes all policies on deferral of… tissue donations that are not based on evidence.” Several organizations, including the American Association of Tissue Banks, American Society of Cataract and Refractive Surgery, and American Society of Transplant Surgeons co-sponsored the AMA resolution and expressed their support for revising the corneal donation policies to align with current scientific evidence.[14, 15]
In November 2021, Dr. Puente worked with his U.S. Congressman Joe Neguse to write a bicameral Congressional letter that was signed by 52 members of Congress and was sent to the director of the FDA and President Biden’s Secretary of Health and Human Services asking for the corneal donation policy to be updated and the public be kept appraised of the progress.[16] Finally, editorials recognizing this issue have arisen in the past year bringing more attention to this important issue.[12, 17] Overall, a multipronged approach has brought us to the progress that has been made today.
The Present
“So much of what we do in medicine is impacted by not the science or medicine but the policy of medicine,” Dr. Michael Puente states.
In May of 2023, the FDA eased their restriction on blood donation by eliminating the time-based deferral system for MSM.[18] Excitingly, on January 30th, 2023, the FDA Center on Biologics announced its intention to review and update its separate policy for corneal donors within the next year.[19] This provides hope to the community fighting to destigmatize corneal tissue donation from otherwise healthy donors. According to Dr. Puente, “If [the governing policy makers] are willing to look at current evidence to change [the blood donation policy] hopefully, they will be willing to see it through for the corneal donation policy as well.” This policy also not only impacts those needing corneal transplants, but also other tissues that can be transplanted such as tendons for orthopedic procedures, skin grafts, and heart grafts.[1]
Why the delay in changing the tissue policy?
“[The reasons are] multifactorial- They felt a lack of urgency. We are one of only a handful of countries that have enough corneas each year to meet our demands…. another factor for the FDA is they were not getting a lot of pressure to change this policy. Gay rights organizations have been lobbying against the blood ban for years, but the advocacy on MSM corneal donation only started a couple years ago,” per Dr. Puente.
The Future
While we have obtained the FDA’s attention on this issue, Dr. Michael Puente encourages students to actively engage with their state medical and ophthalmology societies and participate in events such as the AAO’s Mid-Year Forum. These platforms offer valuable opportunities to gain insights into processes, regulations, and advocacy issues that directly impact medical practice. Dr. Puente emphasizes that policy decisions frequently affect patient care, and emphasizes that “anyone can be the spark to start a campaign” to effect policy change.
References
1. Guidelines for preventing transmission of human immunodeficiency virus through transplantation of human tissue and organs. Centers for Disease Control and Prevention. MMWR Recomm Rep, 1994. 43(Rr-8): p. 1-17.
2. Administration, F.a.D., Guidance for Industry: Eligibility Determination for Donors of Human Cells, Tissues, and Cellular and Tissue-Based Products (HCT/Ps). 2007.
3. Conway, M.D. and M.S. Insler, The identification and incidence of human immunodeficiency virus antibodies and hepatitis B virus antigens in corneal donors. Ophthalmology, 1988. 95(10): p. 1463-7.
4. Schochetman, G., Diagnosis of HIV infection. Clin Chim Acta, 1992. 211(1-2): p. 1-26.
5. Puente, M.A., et al., Association of Federal Regulations in the United States and Canada With Potential Corneal Donation by Men Who Have Sex With Men. JAMA Ophthalmology, 2020. 138(11): p. 1143-1149.
6. Sugar, A. and W.S. Van Meter, Using Data to Rethink the Ban on Cornea Donation From Men Who Have Sex With Men. JAMA Ophthalmology, 2020. 138(11): p. 1150-1150.
7. Singh, R., et al., Corneal transplantation in the modern era. Indian J Med Res, 2019. 150(1): p. 7-22.
8. Gain, P., et al., Global Survey of Corneal Transplantation and Eye Banking. JAMA Ophthalmology, 2016. 134(2): p. 167-173.
9. Banks, C.o.E., Tissue for Corneal Transplantation. 2016.
10. Heck, E., A. Brown, and H.D. Cavanagh, Nucleic acid testing and tissue safety: an eye bank's five-year review of HIV and hepatitis testing for donor corneas. Cornea, 2013. 32(4): p. 503-5.
11. Organization, W.H., Annex 4: guidelines on estimation of residual risk of HIV, HBV or HCV infections via cellular blood components and plasma. WHO Expert Committee on Biological Standardization Sixty-seventh report., 2017. WHO Technical Report Series
12. Whitney Stuard, E.O., Joey Whelihan, Patrick Loehr, Samantha Rea, Bennett Vogt, Phi Luong, Zainab Atiq, Omer Ashruf, Medical Student, Corneal Transplant, Not All the Rules Prevent Blindness. International Journal of Eye Banking 2021. 9(3).
13. Jones JM, K.I., Levi ME, Assessing Solid Organ Donors and Monitoring Transplant Recipients for Human Immunodeficiency Virus, Hepatitis B Virus, and Hepatitis C Virus Infection — U.S. Public Health Service Guideline, 2020. MMWR Recomm Rep 2020(69): p. 1-16.
14. Association, A.M., Blood and Tissue Donor Deferral Criteria H-50.973. Policy Finder 2022.
15. Colorado, A.A.o.O., GLMA: Health Professionals Advancing LGBTQ Equality, American Society of Cataract and Refractive Surgery, Evidence-Based Deferral Periods for MSM Donors of Blood, Corneas, and Other Tissues. America Medical Association House of Delegates, 2021.
16. Release, H.P., Neguse, Cicilline, Quigley, Baldwin, Bennet, Warren, Push FDA to End Discriminatory Tissue Donation Policy. 2021.
17. Medeiros, S., It’s Time to Legalize Gay Eyes. AAO, 2022.
18. Research, U.S.D.o.H.a.H.S.F.a.D.A.C.f.B.E.a., Recommendations for Evaluating Donor Eligibility Using Individual Risk-Based Questions to Reduce the Risk of Human Immunodeficiency Virus Transmission by Blood and Blood Products: Guidance for Industry. FDA, 2023.
19. FDA, Guidance Agenda: Guidance Documents CBER is Planning to Publish During Calendar Year 2023. Biological Guidances, 2023.